Today is World Sickle Cell day (June 19), observed to create awareness about this genetic disorder that impacts the efficiency of the blood. Firstpost brings out a doctor’s view on how to deal with the world’s most monogenic disorder, prevalent in India and sub-Saharan Africa read more
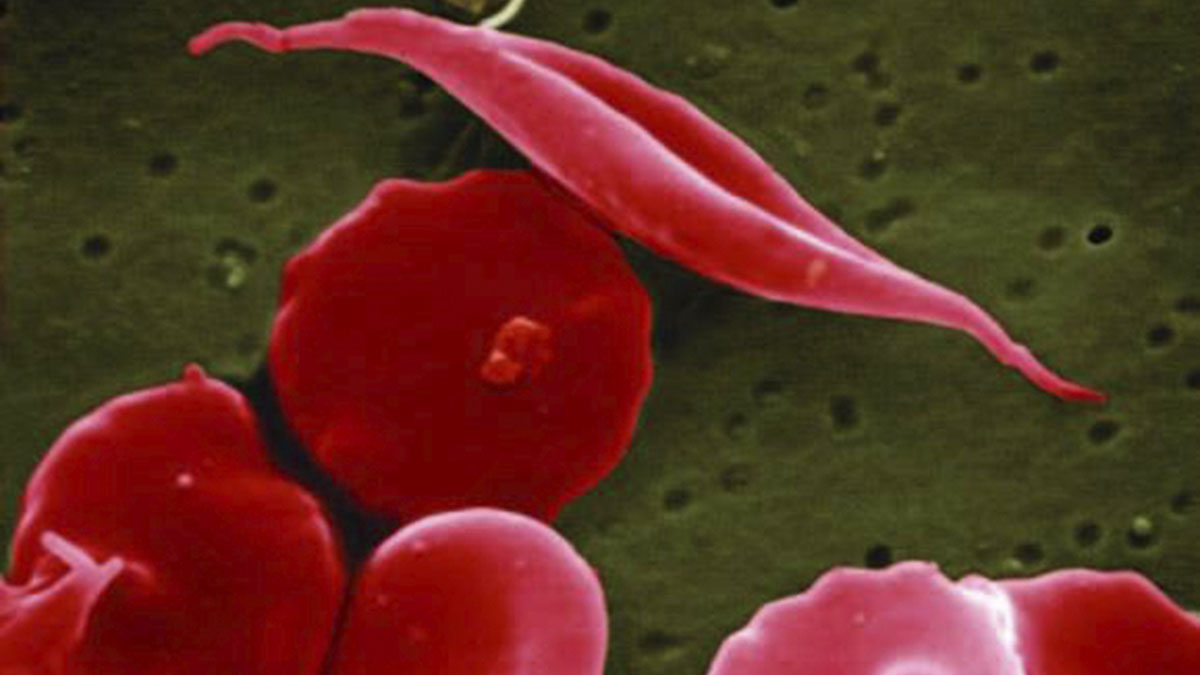)
(File) This electron microscope image provided by the National Institutes of Health shows a blood cell altered by sickle cell disease. AP
Sickle Cell Disease (SCD) is the most common severe monogenic disorder in the world. India accounts for 14.5 per cent of the global SCD newborns, roughly over 42,000 a year, second to sub-Saharan Africa. We spoke to Dr Rahul Bhargava, the principal director & chief of Bone Marrow Transplant (BMT) department at Fortis Memorial Research Institute, Gurugram, Haryana. Excerpts:
What is sickle cell disease (SCD) and how does it affect the body?
Sickle Cell Disease (SCD) is a hereditary blood disorder where the body produces an abnormal form of haemoglobin called haemoglobin S (HbS). Generally, red blood cells are circular and flexible, allowing them to move easily through blood vessels.
However, in SCD, these cells become stiff and crescent-shaped. This irregular shape can cause the cells to cluster and obstruct blood flow, leading to a range of health issues.
Pain crises (vaso-occlusive crises): Blocked blood flow can cause intense pain episodes in the chest, abdomen, and joints.
Chronic haemolytic anaemia: The sickle cells break apart easily and die, leading to a constant shortage of red blood cells.
Infections: SCD weakens the spleen, making the body more vulnerable to infections.
Organ damage: Persistent blockages and anaemia can cause damage to organs such as the spleen, liver, kidneys, lungs, and brain.
Stroke: Blocked blood flow to the brain can result in a stroke.
It is considered the most common severe monogenic disorder in the world. What makes it such an illness?
SCD is considered the most common severe monogenic disorder due to its widespread prevalence and significant impact on those affected. The disorder is caused by a single gene mutation, yet it results in substantial morbidity and mortality. The global burden is particularly high in regions where malaria is endemic, as the sickle cell trait offers some protection against malaria, leading to a higher prevalence of the disease.
What are the genetic causes of SCD, and how is it inherited?
SCD is caused by a mutation in the HBB gene on Chromosome 11, which encodes the beta-globin subunit of haemoglobin. The mutation involves a substitution of valine for glutamic acid at the sixth position of the beta-globin chain, forming HbS instead of normal haemoglobin A (HbA).
SCD is inherited in an autosomal recessive pattern:
Homozygous (HbSS): Individuals with two copies of the HbS gene exhibit symptoms of SCD.
Heterozygous (HbAS): Individuals with one HbS gene and one normal HbA gene are carriers (sickle cell trait) and usually asymptomatic but can pass the gene to their children.
It seems that there is an ethnic or racial vulnerability for SCD. Europe and North America is less affected but sub-Saharan Africa and India are worst affected. Why?
The higher prevalence of SCD in sub-Saharan Africa and India is largely due to the selective advantage of the sickle cell trait in malaria-endemic regions. Carriers of the sickle cell trait (HbAS) have a higher resistance to malaria, which increases their survival rates and, consequently, the frequency of the HbS allele in these populations. Over generations, this evolutionary advantage has led to a higher prevalence of SCD in these regions compared to Europe and North America, where malaria is not endemic.
India accounts for 14.5 per cent of the global SCD newborns, with over 42,000 cases annually. Why is the incidence so high in India?
India’s high incidence of SCD can be attributed to several factors:
Genetic diversity: India’s diverse genetic landscape includes several populations with a high frequency of the HbS gene.
Historical malaria prevalence: Regions historically affected by malaria, particularly central and eastern India, have a higher prevalence of the HbS allele.
Large population: India’s large population size means even a relatively high prevalence rate translates to a significant number of affected individuals.
Endogamous communities: Certain tribal and rural populations practise endogamy (marriage within the same community), increasing the chances of inheriting the HbS gene.
Are there specific populations within India or sub-Saharan Africa that are more affected by SCD?
Yes, certain populations within these regions are more affected by SCD:
India: Tribal groups such as the Gond, Baiga, Bhil, and other Adivasi communities in states like Maharashtra, Madhya Pradesh, Odisha, and Chhattisgarh have higher SCD prevalence.
Sub-Saharan Africa: Countries like Nigeria, Democratic Republic of Congo, and Ghana have high SCD prevalence due to the significant presence of the HbS allele.
What are the common symptoms of SCD? At what age do symptoms typically begin to manifest in children with SCD?
Common symptoms of SCD include:
Pain crises: Sudden and severe pain episodes due to blocked blood flow.
Chronic anaemia: Persistent fatigue and pallor due to the rapid breakdown of red blood cells.
Swelling: Painful swelling in the hands and feet, known as dactylitis.
Frequent infections: Increased susceptibility to infections due to spleen damage.
Delayed growth and puberty: Slower growth rates and delayed sexual maturation.
Vision problems: Damage to the retina from blocked blood flow.
Symptoms typically begin to manifest in children around five to six months of age when foetal haemoglobin (HbF) is replaced by adult haemoglobin (HbS).
How is SCD diagnosed, especially among newborns? Are there any screening programmes in place in high-prevalence areas?
SCD can be diagnosed through:
Newborn screening: Blood tests such as haemoglobin electrophoresis, high-performance liquid chromatography (HPLC), or genetic testing are done to identify HbS.
Prenatal testing: Amniocentesis or chorionic villus sampling (CVS) is used to detect SCD in foetuses.
Many high-prevalence areas have established newborn screening programmes to identify and manage SCD early. These programmes are routine in parts of Africa, India, the United States, and other regions with significant SCD prevalence.
What are the current treatment options available for individuals with SCD?
Treatment options for SCD include:
Pain management: Analgesics, anti-inflammatory drugs, and opioids can be used for severe pain.
Hydroxyurea: Medication that increases foetal haemoglobin (HbF) production, reducing the frequency of pain episodes and acute chest syndrome.
Blood transfusions: Regular transfusions are essential to manage severe anaemia and reduce the risk of stroke.
Bone marrow or stem cell transplantation: Potentially curative but limited by donor availability and the risk of complications.
Gene therapy: Emerging treatment aimed at correcting the genetic mutation causing SCD.
What can be done to fight SCD at the global level?
Yes, lifestyle changes and interventions can help manage SCD symptoms:
Hydration: Drinking plenty of fluids to prevent dehydration and reduce the risk of sickling crises.
Avoiding extreme temperatures: Preventing exposure to very cold or hot environments that can trigger pain episodes.
Regular exercise: Engaging in moderate physical activity to improve overall health without overexertion.
Healthy diet: Maintaining a balanced diet to support overall health and manage anaemia.
Preventive care: Regular vaccinations, prophylactic antibiotics, and routine health check-ups to prevent infections and monitor for complications.
To combat SCD globally, the following actions can be taken:
Expanding newborn screening programmes: Implementing and enhancing newborn screening in high-prevalence regions to ensure early diagnosis and treatment.
Increasing awareness and education: Raising awareness about SCD, its symptoms, and treatment options through public health campaigns.
Enhancing healthcare access: Improving access to healthcare services, including pain management, transfusions, and advanced treatments.
Supporting research: Investing in research to develop new therapies, improve existing treatments, and ultimately find a cure for SCD.
Genetic counselling: Providing genetic counselling to at-risk couples to inform them about carrier status, reproductive options, and the risk of having children with SCD.
These measures can significantly improve the quality of life for individuals with SCD and reduce the global burden of the disease.

 3 months ago
13
3 months ago
13
















)
)
)
)
)
)
)
 English (US) ·
English (US) ·